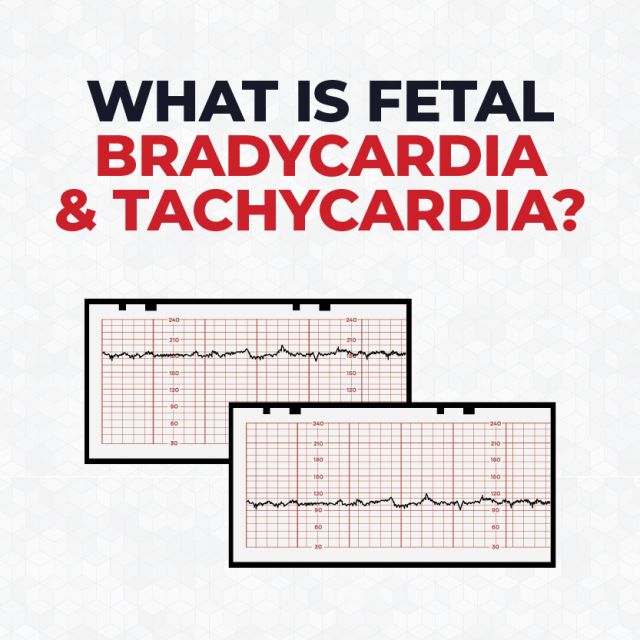
What is Fetal Bradycardia and Tachycardia?
Introduction
A normal fetal heart rate typically ranges between 110 and 160 beats per minute (bpm). However, fetal bradycardia and fetal tachycardia occur when a fetal heart rate drops either below or above this range. These abnormal heart rates can carry significant implications for fetal well-being, requiring electronic fetal monitoring and intervention. In this article, we’ll provide an overview of fetal bradycardia and tachycardia, as well as go over the different types and causes.
What is Fetal Bradycardia?
Fetal bradycardia refers to an abnormally low heart rate in a fetus. Bradycardia is diagnosed when the fetal heart rate drops below 110 bpm for an extended period.
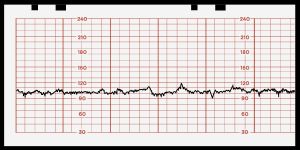
Types of Fetal Bradycardia
There are four types of fetal bradycardia.
- Sinus Bradycardia: A type of fetal bradycardia where the heart rate slows down below 110 bpm, originating from the sinoatrial (SA) node.
- First-Degree Atrioventricular (AV) Block: This type of fetal bradycardia occurs when there is a slight delay in the transmission of electrical impulses between the atria and ventricles of the heart.
- Second-Degree AV Block (Partial Heart Block): In second-degree AV block, some electrical impulses fail to reach the ventricles, leading to occasional missed heartbeats or prolonged pauses in the heartbeat.
- Third-Degree AV Block (Complete Heart Block): This is the most severe type of AV block, where there is complete interruption of the electrical connection between the atria and ventricles.
Causes of Fetal Bradycardia
What is Fetal Tachycardia?
Fetal tachycardia refers to a condition where the fetal heart rate is abnormally high during pregnancy. Tachycardia is diagnosed when the fetal heart rate rises above 180 bpm for an extended period.
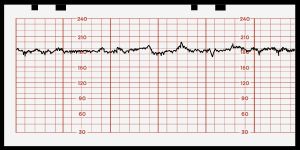
Types of Fetal Tachycardia
There are four types of fetal tachycardia.
- Supraventricular Tachycardia (SVT): SVT is the most common type of tachycardia is characterized by the heart beating faster than 200 bpm.
- Sinus Tachycardia: This type of fetal tachycardia occurs when the heart rate is elevated above 180 bpm, but less than 200 bpm. It’s often associated fever, dehydration, or maternal anxiety.
- Atrial Flutter: Atrial flutter occurs when the rapid heart rate originates from the atria rather than the ventricles, characterized by rapid atrial contractions.
- Ventricular Tachycardia: Ventricular tachycardia occurs when the rapid heart rate originates from the ventricles rather than the atria, characterized by rapid ventricle contractions.
Causes of Fetal Tachycardia
Fetal tachycardia can have various causes. Some of the common factors contributing to fetal tachycardia include:
- Maternal Fever: Maternal fever often results from infections such as urinary tract infections, or viral diseases, which can lead to an increase in the fetal heart rate.
- Fetal Infections: Viral and bacterial infections can cause tachycardia as the fetal heart responds to the stress of infection.
- Maternal Hyperthyroidism: Maternal hyperthyroidism can lead to an increase in maternal circulating thyroid hormones, which may affect fetal heart rate.
- Fetal Anemia: Fetal anemia, low levels of red blood cells in the fetus, can lead to tissue hypoxia that prompt the fetal heart to increase its rate.
- Fetal Distress: Similar to fetal bradycardia, fetal tachycardia can also occur as a response to fetal distress, which may be caused by placental insufficiency, maternal hypertension, or intrauterine growth restriction (IUGR).
Conclusion
As research and technology evolves, our understanding of fetal cardiac abnormalities will evolve as well. By fostering collaboration and using the most advanced fetal monitors, we can strive towards ensuring the best possible prenatal care.